Sciatica
Sciatica is a relatively common condition and a term typically used to describe pain, tingling, numbness or weakness down one leg as far as into the toes. For many, the effect of sciatica symptoms is an everyday battle which immensely impacts the quality of life. Muscle, joint and nerve pain, like the symptoms of sciatica, is one of the most common reasons people visit their primary care physicians, miss time from work, and file for disability.
What it is
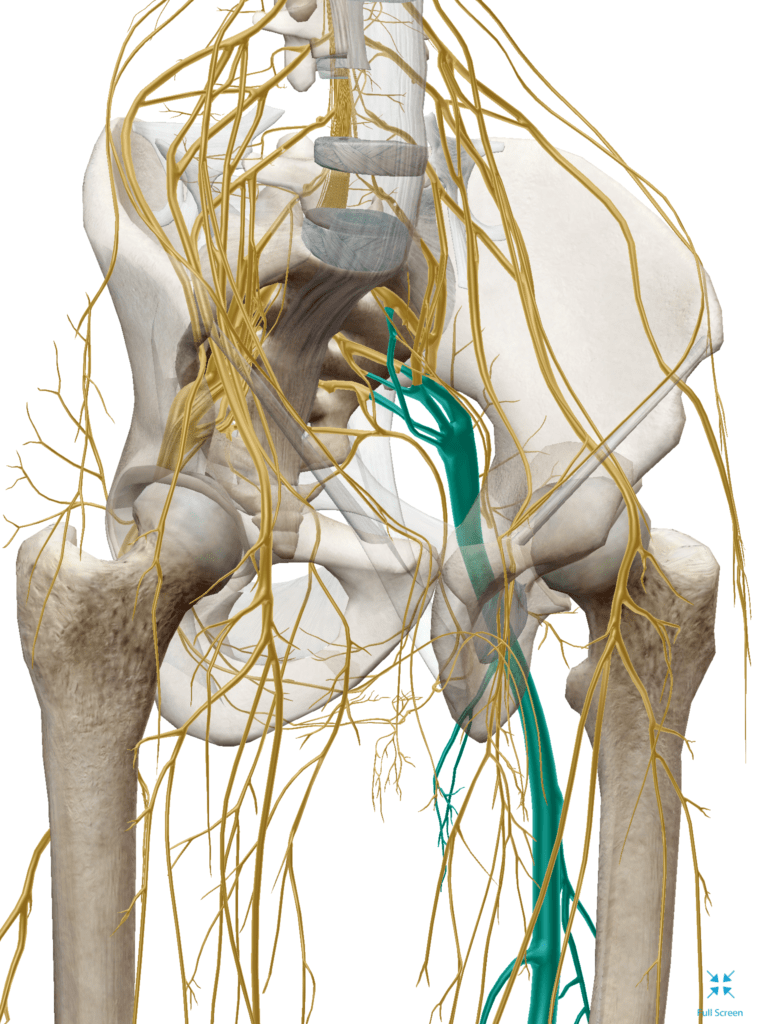
The term “sciatica” refers to pain radiating down the path of the sciatic nerve. The sciatic nerve is a collection of nerve roots exiting both sides of the low back, combining to form the sciatic nerve at hips and buttocks, then travel down each leg. Importantly, just because you have pain in your butt or your legs, does not mean you have sciatica. Make sure to get your problem accurately diagnosed. Pain can be referred down the leg or buttocks from facet joint inflammation or dysfunction, muscle tension or trigger points, sacroiliitis, nerve tension, chemical irritation, and more. Each is treated differently so a proper diagnosis is critical.
Acute sciatica is an episode lasting no longer than six weeks, which is more common than chronic sciatica pain lasting longer than three months.
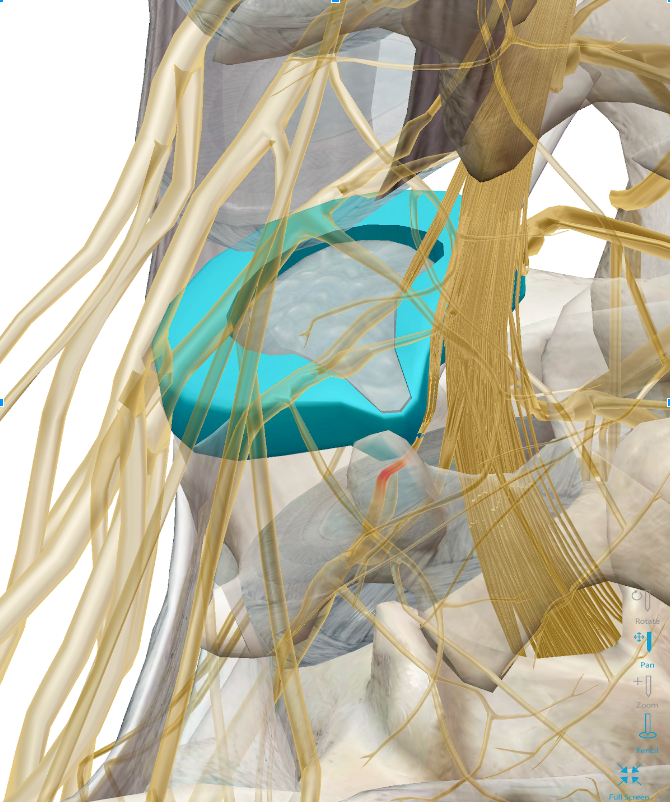
Sciatica occurs when one or multiple nerve roots comprising the sciatic nerve are irritated, pinched, or even compressed. Irritation, pinching, or compression of the nerve roots is commonly thought to be because of a disc bulge or herniation, a boney growth of a spine bone (spinal vertebra bone spur), or more rarely, a tumor or damage from a disease process like diabetes.
Sciatica is most commonly a mechanical problem, meaning an issue occurring as the result of how we use or don’t use our body. If your sciatica pain changes — for better or worse — with varying movement, postures, or positions accompanied by, you likely are suffering from a mechanical low back problem causing sciatica symptoms.
Because the nerve supply to your legs stems from the nerve roots of the spinal cord within the spine, poor spinal mechanics and joint function can alter the signals from your brain to the muscles. And vice versa. Poor muscle function can cause faulty joint motion. Sound like a circle? It’s because it is.
Think of Sciatica as a “kink in the garden hose,” where our nerves are the hose and the water is the information the brain sends to our leg muscles. When the hose is kinked, the full flow of water turns to dribble out the spout. The lack of flow causes an alarm to set off which is sciatica pain and symptoms. Typically, the source of the “kink” is at the level of the spine!
What’s causing the “kink”? It mentioned above, it’s thought to be from disc bulges and bone spurs. However, we’re finding sciatica symptoms can occur with the absence of structural changes, and you can have an identified disc bulge or a bone spur that’s not associated with your sciatica!
Often time the sciatic nerve gets pinched or irritated further down the chain from the spinal canal, as it pierces a muscle caused the piriformis. This is piriformis syndrome. This muscle is in the gluteal region, and through periods of prolonged sitting, can become tight around the nerve, thus “kinking the water hose.” This distinction is important because muscular causes or spinal causes of sciatica are treated differently, making the diagnosis imperative to successful treatment.
In rare cases, sciatica can indicate a serious medical problem requiring immediate attention.
Although most cases of sciatica will resolve on their own without treatment, if you experience constant weakness and numbness of the affected leg, bladder dysfunction, fever, direct trauma, or unexplained weight loss accompanied by sciatica pain, seek immediate medical attention.